Back to: MICROBIOLOGY 300 LEVEL
Welcome to class!
It’s always great to have you back. Today’s topic is one of the most important foundations in microbiology—Gram-positive vs. Gram-negative bacteria. If you’ve ever wondered how scientists tell bacteria apart or why some infections respond differently to antibiotics, this lesson will answer that for you. Understanding the difference between these two major groups of bacteria is like knowing the home and away teams in a football match—it helps you know what strategy to use.
Gram-positive Vs. Gram-negative Bacteria
What is Gram Staining?
Before we look at the differences, let’s talk about Gram staining, the test used to tell the two types of bacteria apart.
The technique was developed by a Danish scientist named Hans Christian Gram in the 1880s. It uses a special dye process to stain bacteria and observe them under a microscope. The results of this test allow us to classify bacteria as either Gram-positive or Gram-negative, based on the structure of their cell walls.
This is not just for show—it helps doctors and microbiologists decide which antibiotics will work and how the bacteria might behave.
Differences Between Gram-Positive and Gram-Negative Bacteria
Let’s break it down simply:
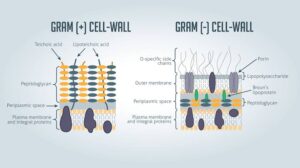
1. Cell Wall Structure
Gram-positive bacteria have a thick peptidoglycan layer (a strong mesh-like structure) in their cell wall.
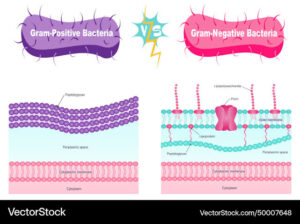
Gram-negative bacteria have a thin peptidoglycan layer but an extra outer membrane made of lipopolysaccharides (LPS), which makes them harder to kill.
2. Gram Stain Reaction
Gram-positive bacteria retain the purple dye (crystal violet) and appear purple under the microscope.
Gram-negative bacteria lose the purple dye and take up a red or pink stain (safranin), so they appear pink.
3. Resistance to Antibiotics
Gram-positive bacteria are generally more sensitive to antibiotics like penicillin.
Gram-negative bacteria are more resistant due to their outer membrane, which acts like a shield.
4. Toxins
Gram-positive bacteria mostly produce exotoxins—proteins that are secreted and can cause disease even in small amounts.
Gram-negative bacteria produce endotoxins—parts of their outer wall that can trigger strong immune responses when the bacteria die.
5. Examples
Gram-positive bacteria: Staphylococcus aureus, Streptococcus pneumoniae, Bacillus anthracis (anthrax).
Gram-negative bacteria: Escherichia coli, Salmonella typhi, Neisseria gonorrhoeae.
Let’s use a Nigerian market example. Think of Gram-positive bacteria like traders inside open shops with just thick walls—they’re easier to reach and interact with. Gram-negative bacteria are like traders inside a gated compound with an extra layer of security—you need more effort or different tools (antibiotics) to get in.
Why Does This Matter?
In diagnosing infections: Gram staining gives quick results.

In treatment: Knowing if a bacterium is Gram-negative or positive helps the doctor choose the right antibiotic.
In public health: Gram-negative bacteria often cause more severe infections due to their resistance and toxin release.
Summary
- Gram staining separates bacteria into Gram-positive (purple) and Gram-negative (pink) based on cell wall structure.
- Gram-positive bacteria have thick peptidoglycan walls and no outer membrane, while Gram-negative bacteria have thin walls and a protective outer membrane.
- These differences affect their appearance, behaviour, and response to antibiotics.
Evaluation
- What is the main difference in the cell wall structure of Gram-positive and Gram-negative bacteria?
- Why do Gram-negative bacteria appear pink under a microscope after Gram staining?
- Give two examples each of Gram-positive and Gram-negative bacteria.
This knowledge is part of what sets you apart as a microbiologist-in-training. You’re gaining the skills to make smart decisions in the lab and in health care settings. Keep showing up and stay curious—Afrilearn is proud to support your journey every step of the way. See you in the next class!
