Back to: MICROBIOLOGY 100 LEVEL
Welcome to class!
It’s a joy to have you here again. You know, your dedication to learning is exactly the kind of energy that changes the world—one smart decision at a time. Today, we’re building on what we learned in our last lesson. So, get comfy, grab your learning gear (your brain and a pen), and let’s get started.
Resistance Mechanisms
Imagine a burglar trying to break into a house, but the house has upgraded its doors, windows, and even set up a security system. No matter what the burglar tries, nothing works. That’s exactly how bacteria behave when they develop resistance to antibiotics—they upgrade their defences to fight off what used to kill them.
Bacteria are very clever little organisms. When exposed to antibiotics, some of them develop resistance, not because they hate medicine, but because they want to survive. Let’s go through the major mechanisms they use to fight back.
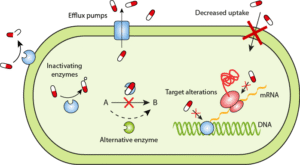
1. Enzymatic Degradation or Modification
This is like having a pair of scissors that cuts up your enemy’s weapon before they can use it. Some bacteria produce enzymes that destroy the antibiotic before it can do any harm.
Example: Bacteria that produce beta-lactamase break down penicillins and cephalosporins before they can damage the bacterial cell wall. It’s like pouring water on a fire before it even starts burning.
2. Alteration of Target Sites
Think of a key and a lock. If bacteria change the shape of the “lock” (their target site), then the antibiotic “key” won’t fit anymore. So, the drug becomes useless because it can’t attach and work on the bacteria.
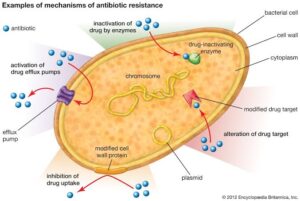
Example: Some bacteria change their ribosomes (where proteins are made), so antibiotics like macrolides can’t bind effectively.
3. Efflux Pumps
These work like water pumps, but instead of removing water, they push antibiotics out of the bacterial cell. So, even if the drug enters the cell, it’s quickly kicked out before it can do any damage.
Example: Tetracycline resistance often happens this way. The bacteria eject the antibiotic right after it enters.
4. Reduced Permeability
Sometimes bacteria change their outer walls so that antibiotics can’t even enter. Imagine locking your gate and refusing to let any strangers in. No entry means no effect.
Example: Some gram-negative bacteria modify their porin channels (protein gateways), blocking antibiotics like carbapenems.
5. Bypass Pathways
Bacteria are also smart enough to find alternative ways to survive. If an antibiotic blocks one path, they create a new one!
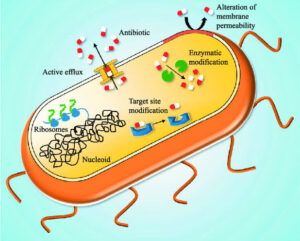
Example: Some bacteria can make folic acid using a different method, so even when sulfonamides block the usual pathway, the bacteria still grow.
Summary
- Bacteria use resistance mechanisms to survive against antibiotics.
- These mechanisms include:
- Producing enzymes that destroy or modify antibiotics.
- Changing the antibiotic’s target site inside the bacteria.
- Using efflux pumps to push the antibiotic out.
- Blocking antibiotic entry by altering their cell walls.
- Creating alternate biochemical pathways to continue functioning.
- These tricks help bacteria stay alive even when antibiotics are present, making infections harder to treat.
Evaluation
- What does the enzyme beta-lactamase do in resistant bacteria?
- Explain how efflux pumps contribute to antibiotic resistance.
- Give two other resistance mechanisms bacteria use, and explain each with an example.
Every lesson you complete brings you one step closer to mastery. Afrilearn is so proud to be part of your journey. Keep asking questions, stay curious, and never forget—you were made for greatness. Let’s keep the fire of learning burning. See you in the next class!
